There are many pathologic changes that may occur in the Achilles’ tendon. Tendinosis, indicating abnormal pathology or degeneration of the tendon, can be insertional (where the tendon attaches to the heel bone), or non-insertional and acute rupture of the tendon, are common conditions that may require operative intervention
INSERTIONAL TENDINOSIS (Haglund’s Deformity)
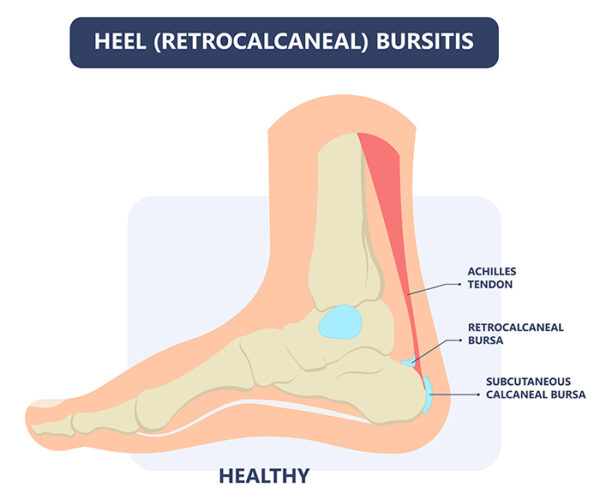
inflammation of the Achilles’ tendon where it inserts into the calcaneus (heel bone) is known as insertional tendinosis. It is often associated with an abnormal bony prominence just deep to the tendon known as Haglund’s deformity or pump bump. The insertion of the Achilles can also calcify adding to the bump. This may play a role in rubbing on the deep aspect of the tendon to cause pain and inflammation in the tendon and surrounding soft tissues. If large enough, it can also rub on footwear or even prevent the wearing of certain shoes.
Non-Operative Management
Initial management of this condition includes activity modification/rest, ice, stretching exercises, anti-inflammatories, and heel lift orthoses. A medial arch support may be of assistance by decreasing over-pronation that may exacerbate symptoms. Corticosteroid injections should be avoided due to increased risk of tendon rupture
Operative Management
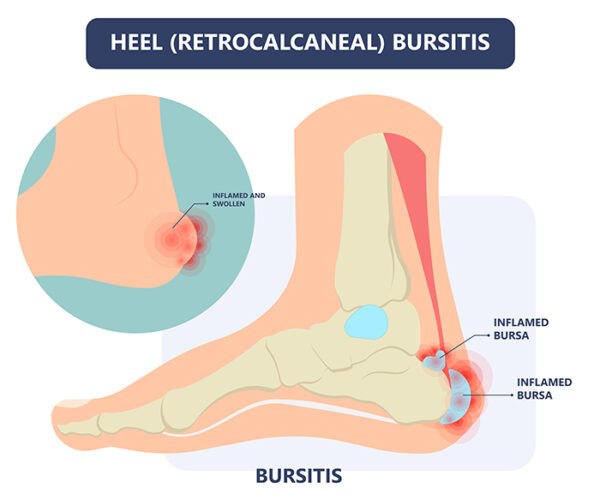
The form of operative management is dependent on the degree of involvement of the Achilles’ tendon. When the tendon is significantly involved, or if the Haglund’s deformity is too large. This involves incisions next to the tendon. The bursa (fluid containing sack deep to the tendon that will also be inflamed) is firstly excised, followed by the Haglund’s deformity. This allows removal of diseased tissue from within the Achilles’ tendon, safe excision of a large deformity, and repair of the tendon to the calcaneal bone.
NON-INSERTIONAL TENDINOSIS
Non-insertional tendonitis is inflammation in and around the Achilles’ tendon higher up the leg from the heel. It most commonly occurs in association with running and jumping sports where forces in the Achilles’ tendon can increase to 10 times body weight. It can also occur in association with overuse syndromes, postural problems, poor footwear, or an underlying inflammatory condition that may affect multiple joints in the body. Patients usually experience pain approximately 2-6 cm further up the leg from the heel. This may even occur at rest and/or at night. Over time, the tendon becomes thickened and an abnormal lump may be felt in the same area. Non-Operative Management Initial management is similar to that of insertional tendinosis. A Stretching exercises of calf muscles, shock wave therapy may also be advised. If symptoms have gone on longer than 6 months, this condition becomes very difficult to manage non-operatively as the tendon will have started to degenerate. Accordingly, when non-operative measures have failed or more than 6 months has elapsed, operative management is indicated. surgery involves That the diseased tendon and surrounding tissue is removed and the remaining healthy tendon is refashioned to bridge the defect. Additionally
ACUTE ACHILLES’ TENDON RUPTURE
Rupture of the Achilles’ tendon may follow a prodromal phase of tendonosis (latent tendonitis). The actual inciting event however, is usually mechanical stress with a rapid loading of an already-tensed tendon, e.g. lunging forward from a standing start, unexpected stepping in a hole, or jumping from a height. Whatever the cause, patients often describe a sudden pain likened to being kicked in the back of the ankle/lower leg, which may be accompanied by an audible pop. Non-Operative Management Non-operative management involves placing the leg in a below knee cast with the toes pointed. This cast is changed every 2 weeks until the ankle is finally in neutral. This process takes approximately 8 weeks. Due to the morbidity and associated high re-rupture rate (18%), this technique is usually reserved for patients who are at high risk of complications from surgery from either an anaesthetic or surgical point of view. The later includes people who smoke or have diabetes, due to their increased risk of wound breakdown and infection. Operative Management: An operation involves an incision at the back of the leg, and the two tendon ends are sutured back together. rarely occasionally a strong direct repair is not possible due to significant damage in the tendon upon rupture. In this situation, a spare tendon in the back of the leg or hamstring tendon may be required to augment the repair.