Osteomyelitis – Adult
- Summary
- Osteomyelitis is the infection of bone characterized by progressive inflammatory destruction and apposition of new bone.
- Diagnosis requires careful assessment of radiographs, MRI and determining the organism via biopsy and cultures.
- Treatment is often a combination of culture-directed antibiotics and surgical debridement of nonviable tissue.
- Epidemiology
- Incidence
- the exact incidence is unknown
- Risk factors
- recent trauma or surgery
- immunocompromised patients
- poor vascular supply
- systemic conditions such as diabetes and sickle cell
- peripheral neuropathy
- Incidence
- Timing classification
- acute
- within 2 weeks
- subacute
- within one to several months
- chronic
- after several months
- acute
- Symptoms
- pain
- fever
- more common in acute osteomyelitis
- Physical exam
- vital signs
- fever, tachycardia, and hypotension suggest sepsis
- inspection
- motion
- limp and/or pain inhibition with weight-bearing or motion may be present
- assess the joints above and below the area of concern
- neurovascular
- assessment of vascular insufficiency locally or systemically
- vital signs
- Imaging
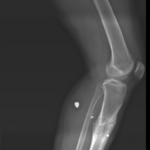
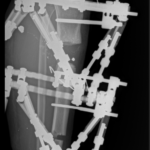
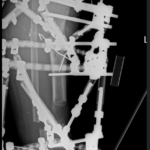
- Radiographs
- findings
- sensitivity and specificity is variable
- CT
- indications
- assist in diagnosis and surgical planning by identifying necrotic bone
- sensitivity and specificity may be affected by hardware artifact and scatter
- indications
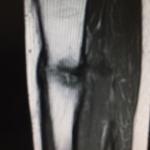
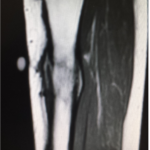
- MRI
- indications
- assists in the diagnosis and surgical planning
- best test for diagnosing early osteomyelitis and localizing infection
- indications
- Nuclear medicine
- Radiographs
-
-
-
- indications
- when radiographs are normal and MRI is not an option
- sensitivity and specificity
- highly sensitive but not specific
- if negative rules out osteomyelitis
- indications
-
-
- Studies
- Laboratory analysis
- leukocyte count (WBC)
- only elevated in 1/3 of acute osteomyelitis
- erythrocyte sedimentation rate (ESR)
- usually elevated in both acute and chronic osteomyelitis (90%)
- a decrease in ESR after treatment is a favorable prognostic indicator
- usually elevated in both acute and chronic osteomyelitis (90%)
- C-reactive protein
- most sensitive test with elevation in 97% of cases
- decreases faster than ESR in successfully treated patients
- most sensitive test with elevation in 97% of cases
- blood cultures
- often negative, but may be used to guide therapy for hematogenous osteomyelitis
- leukocyte count (WBC)
- Microbiology
- sinus tract cultures
- not reliable for guiding antibiotic therapy
- culture of bone
- gold-standard for guiding antibiotic therapy
- sinus tract cultures
- Laboratory analysis
- Treatment
- Goals
- success in the treatment is dependent on various factors
- patient factors
- immunocompetence of patient
- nutritional status
- injury factors
- the severity of the injury as demonstrated by segmental bone loss
- infection location
- other factors affecting prognosis and treatment include:
- residual foreign materials and/or ischemic and necrotic tissues
- inappropriate antibiotic coverage
- lack of patient cooperation or desire
- patient factors
- success in the treatment is dependent on various factors
- Nonoperative Treatment
- suppressive antibiotics
- indications
- when operative intervention is not feasible
- indications
- suppressive antibiotics
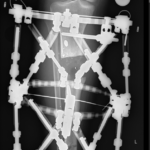
- Operative treatment
- irrigation and debridement followed by organism-specific antibiotics
- indications
- acute osteomyelitis that fails to improve on IV antibiotics
- subacute osteomyelitis
- abscess formation
- chronic osteomyelitis
- draining sinus
- indications
- irrigation and debridement followed by organism-specific antibiotics
- Goals
- Techniques
- Antibiotic therapy
- technique
- antibiotics should be tailored to a specific organism, preferably after a bone biopsy is obtained
- chronic suppressive antibiotics may be useful in patients who are immunocompromised or in whom surgery is not feasible
- high rates of recurrence if suppressive antibiotics are discontinued
- technique
- Irrigation & Debridement
- soft tissue
- all devitalized and necrotic tissue should be removed
- extensive debridement is essential to eradicate the infection
- bone work
- sequestrum must be eliminated from the body, or infection is likely to recur
- debride bone until punctate bleeding is seen – “paprika sign”
- hardware removal
- any non-essential hardware should be removed
- dead space management
- instrumentation
- outcomes
- often requires a staged approach with multiple debridements and delayed soft tissue coverage
- when combined with postoperative antibiotics tailored to a specific organism, treatment is often successful
- soft tissue
- Antibiotic therapy